kidney Disease and Diabetes
You are at risk of developing chronic kidney disease if you suffer from type 1 or type 2 diabetes. Diabetic nephropathy is a condition where the kidneys become damaged overtime due to uncontrolled diabetes.
When your diabetes is uncontrolled due to practices like unhealthy eating habits, not taking medication as prescribed and not self-monitoring glucose levels, this can have a severe effect on the kidneys over time. Uncontrolled diabetes can cause damage to the small blood vessels of the kidneys that filter waste, toxins and excess fluids from the blood leading to kidney damage.
According to the Centre for disease control “Each kidney is made up of millions of tiny filters called nephrons. Over time, high blood sugar from diabetes can damage these blood vessels in the kidneys so they don’t work as well as they should. Many people with diabetes also develop high blood pressure, which can damage kidneys too”.
You are at risk of developing diabetic nephropathy is you have diabetes and your blood glucose is too high and if your blood pressure is too high. You are also at risk if you don’t follow your diabetic eating plan, eat foods high in salt, do not exercise, are overweight, have heart disease and have a family history of kidney disease.
You can help to reduce your risk of diabetic nephropathy by managing your diabetes effectively, including seeing a nutritionist or dietician for advice on healthy eating habits to help you manage your blood sugar and blood pressure.
Chronic Kidney Failure (What it is)
The kidneys are two bean-shaped organs that filter blood, removing wastes, toxins, and excess fluids through urine. If your kidneys are damaged and cannot perform this task effectively, these waste, toxins and excess fluids build up in the body, makes you sick and can be fatal if not treated. The body can function adequately with one kidney once that kidney functions properly.
Chronic Kidney disease or renal failure occurs when one or both of the kidneys are unable to perform their duties adequately. You are at risk of developing chronic kidney disease or renal failure if you have chronic diseases like diabetes, hypertension, cardiovascular disease, or other problem with the heart. You are also at risk for kidney disease if you are obese or have a high body mass index, have a family history of kidney disease, if you are over the age of 60 and if you smoke. There are other conditions that can also lead to kidney damage such as, lupus, enlarged prostate and kidney stones.
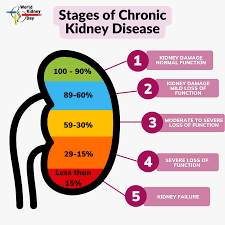
Early diagnosis and treatment of chronic kidney disease can help slow the progression from mild damage which is stages 1 and 2, to severe damage of the kidneys which is stages 3 to 5, that can lead to kidney failure which is fatal without dialysis or transplant. The first two stages of kidney failure may not present symptoms as in stage 1 the kidneys are still filtering at a high level with mild damage, while in stage 2 the filtration rate is decreased but still, may not be significant enough to produce symptoms. If you do experience symptoms, they may be nonspecific such as swollen hands, feet, frequent need to urinate especially at night, and blood in urine. Managing conditions like diabetes and high blood pressure are important at these two stages.
Stage 3 chronic kidney disease presents with a mild-to-moderate decrease in kidney function, this is when the kidney is not able to filter fluids, waste, and toxins as it used to, causing them to build up in the body. This is most often the stage when people are diagnosed with chronic kidney disease. Symptoms include persistent itching, back pain, urinating more or less than usual, problems sleeping, and tiredness. Implementing a kidney specific diet and nutrition plan at this stage can help to reduce symptoms and slow disease progression. This plan normally includes reducing the intake of sodium and protein and may include adjustments in potassium based on your blood levels.
In stage 4, there is severe decrease in the kidneys’ ability to filter, and the buildup of waste, toxins, and fluids in the body is increased. The diet plan will remain with control of protein, and sodium; adjustments of potassium, phosphorus, and calcium, will be suggested by your doctor and nutritionist; regular testing will allow better dietary monitoring and timely adjustments of diet and medications. Your intake of fluids may be limited if you are retaining fluids. Medications and dietary management can help in delaying the progression to stage 5, which is End Stage Kidney Disease, with very little kidney function left or kidney failure. Dialysis or transplant will become necessary as a means of clearing waste and extra fluids from your body.
An early diagnosis of Kidney or renal disease can be done through urine and blood tests. These tests can check if you are losing protein in your urine and an estimated glomerular filtration rate test is a blood test that checks how well the kidneys are filtering. It is important to get annual general medical check-ups to monitor the function of the body’s organs, even if you are feeling well.